 Some data from New York City
Some data from New York City
Introduction
The following analysis and write-up was done by dcleve. I appreciate the time and effort he put into writing this up. I corrected a couple of typos but and did a bit of formatting, but I did not research or write this. My thanks to dcleve for taking the time to lay this out.
 Unhappy lungs
Unhappy lungs
The analysis
This is my effort to figure out where we are with Covid-19, without doing exhaustive research.
The summaries available from the CDC are vague, and US data appears poor due to limited testing, and deliberate underreporting. To get better understanding, I looked to overseas reports.
So – what is the risk from the disease? It has a moderate death rate, and is a dangerous disease, to people in every age group. But the risk increases with age. Also, there are multiple reports of long term health consequences in survivors. So both death and disability are risks.
The risk of death is skewed in many reports in three ways: by under-reporting of infections, by under-reporting of deaths caused by the disease, and by snap-shot reports before the ill people have either died or recovered. The best data on total fatality rate would come from a country which tested a lot, and reported tests accurately, and has pretty much beaten the disease. I looked at New Zealand, which had a 2% fatality rate, and S. Korea, which had a 2.4% fatality rate, as the best data sources.
The most useful breakdown of death rate by age I could find was from China.
Here is a link to the Chinese fatality rate data by age, showing the risk of death if one gets infected. This Chinese study showed an overall death rate of 2.25%, with men ~1% more at risk than women (~2.75% vs 1.75% death rates). With the average from China matching the more recent data from New Zealand and S Korea, this seems like trustworthy data.
There is some additional useful data in this Chinese study about the effect of pre-existing conditions. Long-term health concerns like diabetes and cancer increased individual risks to between 6-10%. The risk of death to those without health complications was ~0.9%. So, this table can be adjusted by ~3X up for those with pre-existing conditions, and down by ~2X for those without.
However, as a statistics caveat, older patients almost all have health complications, so the oldest patient data likely tend to mix these two effects, and these multiplication rates would give inaccurate predictions for the top two categories. I will take my own guess at this in my own table below.
Death, unfortunately, is not the only risk. As I noted earlier, a significant number of survivors have major organ damage post-recovery, the most common being significant lung scarring, and strokes. I was not able to find much in the way of statistics on this. One of the few sources I found was
a UK estimate reported by Vox:
"The UK National Health Service assumes that of Covid-19 patients who have required hospitalization, 45 percent will need ongoing medical care, 4 percent will require inpatient rehabilitation, and 1 percent will permanently require acute care."
I am treating all “need ongoing medical care” as long term effects. This is per “hospitalized” patients, which I couldn’t find a good estimate on. I tried piecing together bits of data to figure this out: China reported 5% of cases were severe -- and 13% had significant symptoms -- it is not clear how either of these relate to hospitalization rates in the UK, but one can assume UK hospitalization is at least 5%. Using my 2.25% overall death rate estimate, if 5% hospitalization ==> 2.25% death rate, and 45% of the 5% need ongoing care, which is also 2.25%, then the rate of post-recovery injury is about equal to the death rate.
If I assume that severe symptoms track with age the same rate the deaths track with age, then , if one cares about BOTH death OR long-term injury, one can double the death rate numbers for Italy to come up with health risk.
Here is my best estimate table:
Age Average health risk (death or long-term health issues) Risk without preconditions Risk with preconditions
80+ .........29.6% ..... 7.5%*..... 44%*
70-79 ......16.0% ..... 4.5%* .... 27%*
60-69 ......7.2% ....... 2.5%* .... 15%*
50-59 ..... 2.6% ....... 1.0%* .... 6%*
40-49 ..... 0.8% ....... 0.3% ...... 2.5%
10-39 ..... 0.4% ....... 0.15% .... 1.25%
Overall average 4.5%
Note, * is my guestimated adjustment to decouple age and preconditions
Note, there is risk in every age group, even among the healthy. A 0.15% risk for younger healthy people is a risk that most would not like to take – it is one death or disability for every 667 people who catch the disease. As a check – this is about the rate seen in the US aircraft carrier – one death in ~800 cases.
How is COVID-19 transmitted? Early studies focused on contact transmission – COVID-19 was found on computer mice, door handles, etc in hospitals. This IS a way it can be transmitted. But there has been a lot of evidence for a while that airborne transmission is the greater risk. The spread in cruise ships, even when passengers were in lockdown, shows it can go through ventilation systems. But the lack of spread within the apartment buildings locked down in China shows that larger spaces and better filtration than on ships can limit its spread inside a building. The lower rate of spread in east Asia, where people wear facemasks, vs the US and Europe, shows facemasks help. When New York and Italy imposed face mask requirements on their populations, in ADDITION to social distancing, they both turned the corner on the disease.
How to stop the disease: the strongly controlling countries of China, Taiwan, Japan, S Korea, N Zealand, and Australia have almost eliminated COVID, because they were willing to mandate extreme measures, country-wide.
The US government has not set policy in the US -- the initial lockdown was initiated by sports leagues, and then the implementation of mandatory restrictions has been an uneven patchwork state-state. And none of our state mandates have even remotely approached what the successful countries noted above have done. This is why the US leads the world in COVID deaths.
Reopening an economy only makes sense if the COVID infection rate has been brought under control, so that normal behaviors do not carry a high risk of infection. This is what the successful countries above have done, and they are opening safely. They did not reopen until the "curve" had almost re-hit zero. If the undiagnosed COVID infection rate in the country were only a few thousand, and we had tracing, the US could open safely. We instead have millions of undiagnosed cases, so full re-opening will just lead to an even more massive infection rate nationwide.
The states which have reopened anyway, have seen an increase in COVID rates. By reopening before taming this disease, they insure they will never get a "second wave" because they will never end the "first wave".
Enough individuals have noticed the difference between effective responses and the US response, and self-imposed more extreme personal behavior, that the US death and infection rates have not been nearly as bad as they could have been. This is particularly true for "reopening", where we have not seen the massive increase in infections that one would expect. This is BECAUSE so many people are not listening to their governments, and are instead trying to personally apply more stringent transmission control, to minimize their own risks of catching COVID-19. Self-protection like this, while officially re-opening, will pretty much insure a long-term economic recession, as a significant fraction of the population tries to save their lives and health.
Long-term: The demonstratedly successful long-term approach is for the US to re-impose strict national controls, but this time with masks, testing and contract tracing. This brought the disease under control in China, even thought it was initially widespread. And it worked in most of the countries around China.
A second long-term solution would be if we develop a vaccine. Widespread vaccination would end this threat. The earliest plausible dates I have seen for a good vaccine to have been shown effective are Jan-Feb of next year, which would then need to be followed by mass production and distribution, which would take months more. The earliest I think mass vaccinations are possible would be ~1 year from now. However, there have been some diseases where developing a vaccine took up to 30 years, so ~1 year to get a vaccine may be wildly optimistic.
The US policy is effectively "spreading the curve" -- distributing deaths over months and years, so that morgues are not overwhelmed. The curve would not be spreading if individuals were not exceeding state guidelines, we would instead be seeing a massive infection spike. Spreading the curve could eventually bring this infection under control through herd immunity, which needs ~80% of the population to have gotten the disease. The rational choice under a "spread the curve" policy, is to over-protect oneself, letting the rest of the population get the disease and its risk of death or debilitation, then only re-engage society after herd immunity brings levels of infection under control.
How long this would take depends on how successful people are at preventing the spread though personal protective measures. There are not very many random tests of the population to see what the infection rate nationwide has been. One recent random study in Indiana showed a 2.8% infection rate as of May. If one extrapolates this out to the US population, we are currently under 5%.
If our rate of spread is ~1% per month, it would take ~75 more months for us to get to herd immunity IE~6 years. (emphasis added by me)
Personal protection if disease is untamed: The worst infection rates have occurred indoors when people are in close proximity. Cloth or simple paper facemasks and hand sanitizer help, but with long-term exposure in hospitals, the staff still suffer from significant infection rates. If one has to go indoors, exposure time seems to matter. Quick trips indoors are lower risk, while long exposure indoors is of greater risk. For longer term exposure, the meat packing plants with their high transmission rate show that masks alone do not stop the disease fully, and that social distancing plus masks helps. The cruise ship results, with the disease traveling between small cabins, show that infection can occur at greater than 6-ft “social distance” separation, and any additional distance above 6-ft is also helpful.
Personal protection should therefore be to avoid possible infection circumstances (proximity to those not in one’s household, or being indoors outside one’s household) as much as possible, and always wearing masks, and regularly hand sanitizing.


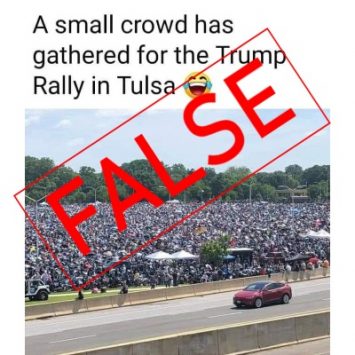 Trump Rally in Tulsa
Trump Rally in Tulsa 



